Lung Nodule Detection Is Getting Smarter
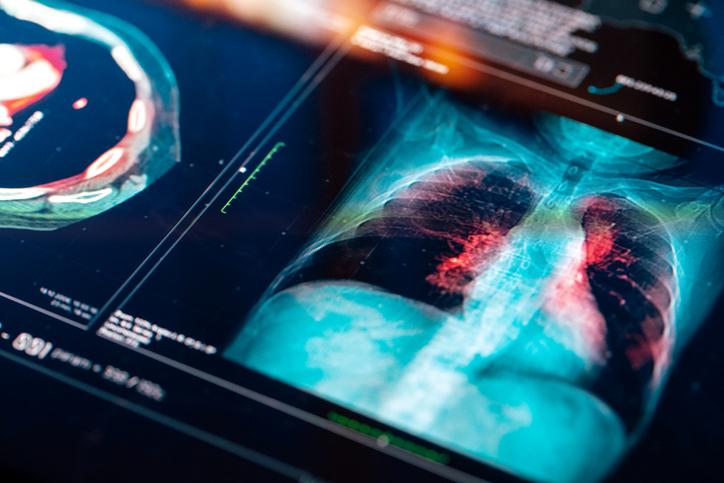
A new deep learning model is changing how doctors evaluate lung nodules found on CT scans. These nodules are small growths that may or may not be cancerous. The difficulty lies in identifying which ones need urgent attention and which can be safely observed over time.
Standard tools like the PanCan model rely on patient information and visible features. But these tools often fall short, especially when nodules fall in the indeterminate size range of 5 to 15 millimeters. That’s where this new AI model makes a difference.
The Risk of Guesswork in Lung Scans
Many people who undergo CT scans are told they have a lung nodule. While most are harmless, some develop into cancer. The biggest challenge is accuracy. If a nodule is wrongly classified as high risk, the patient may face stressful and unnecessary biopsies. If cancer is missed, the delay in treatment can lower survival odds.
This new deep learning tool uses advanced image recognition to make more accurate predictions than traditional methods. It evaluates patterns in the scan that go beyond what the human eye or clinical models can detect.
Why the AI Model Performs Better
In clinical testing, the deep learning model showed stronger results across several groups of patients. It was especially effective with nodules between 5 and 15 millimeters. These cases are typically the hardest to judge.
The model also performed well in difficult comparisons, such as when cancerous and noncancerous nodules are similar in size. It was better at correctly identifying both high-risk and low-risk cases. This means fewer false alarms and fewer missed cancers.
When used at full sensitivity, the model identified all confirmed cancers within one year while lowering the number of benign nodules flagged for follow-up. Fewer patients were told to return for more tests when it wasn’t necessary.
A Step Toward Better Care and Fewer Procedures
Doctors aim to catch cancer early without putting patients through needless procedures. This model could help strike that balance. By reducing false positives, it may lead to fewer follow-up scans, fewer invasive biopsies, and less anxiety for patients.
It also supports better conversations between doctors and patients. When the risk is clearer, the next steps can be more confidently chosen. That could mean continued observation or a decision to take action based on real evidence.
Where This Model Could Be Used
This kind of deep learning system may eventually be used in lung cancer screening programs, especially for high-risk individuals like smokers or people exposed to asbestos. Radiologists might use it alongside standard tools to evaluate nodules more accurately and make quicker, more confident decisions.
Before that happens, the model will need further testing in larger and more diverse populations. Clinical validation and integration into medical software are also required before it becomes a routine part of patient care.
Frequently Asked Questions
How is this AI model different from traditional methods?
It analyzes the CT scan directly using deep learning, which allows it to detect subtle patterns that existing clinical models may miss.
Will this replace radiologists or other cancer risk models?
No. It is meant to work alongside radiologists and tools like the PanCan model to improve decision-making, not replace it.
Does it work for all lung nodules?
The model works best for nodules between 5 and 15 millimeters in diameter, where risk is harder to assess using traditional methods.
Can this model reduce unnecessary procedures?
Yes. It lowers the number of false positives, which may reduce the number of follow-up scans, biopsies, and unneeded treatments.
Is this model being used in hospitals now?
Not yet. It is still in the research phase and must be validated in future clinical studies before it becomes widely available.
How will this help patients long term?
Patients may benefit from earlier cancer detection, fewer unnecessary procedures, and clearer guidance about their care plan.
